J. Cent. South Univ. (2016) 23: 1208-1214
DOI: 10.1007/s11771-016-0370-y

Recommendation application for video head impulse test based on fuzzy logic control
NGUYEN Thi Anh Dao1, KIM Dae Young2, LEE Sang Min3, KIM Kyu Sung2, Seong Ro Lee4, KWON Jang Woo1
1. Department of Computer and Information Engineering, Inha University, Incheon, 402-751, Korea;
2. Department of Otorhinolaryngology, Inha University Hospital, Korea;
3. Department of Electronic Engineering, Inha University, Incheon, 402-751, Korea;
4. Department of Information and Electronics Engineering, Mokpo National University, Korea
 Central South University Press and Springer-Verlag Berlin Heidelberg 2016
Central South University Press and Springer-Verlag Berlin Heidelberg 2016
Abstract:
Vestibulo-ocular reflex (VOR) is an important biological reflex that controls eye movement to ensure clear vision while the head is in motion. Nowadays, VOR measurement is commonly done with a video head impulse test based on a velocity gain algorithm or a position gain algorithm, in which velocity gain is a VOR calculation on head and eye velocity, whereas position gain is calculated from head and eye position. The aim of this work is first to compare the two algorithms’ performance and to detect covert catch-up saccade, then to propose a stand-alone recommendation application for the patient’s diagnosis. In the first experiment, for ipsilesional and contralesional sides, the calculated position gain (0.94±0.17) is higher than velocity gain (0.84±0.19). Moreover, gain asymmetry of both lesion and intact sides using velocity gain is mostly higher than that from using position gain (four out of five subjects). Consequently, for subjects who have unilateral vestibular neuritis diagnosed from clinical symptoms and a vestibular function test, vestibular weakness is depicted by velocity gain much better than by position gain. Covert catch-up saccade and position gain then are used as inputs for recommendation applications.
Key words:
vestibulo-ocular response; video head impulse; velocity gain; position gain; desaccade;
1 Introduction
Vestibular-ocular reflex (VOR) is one of three important reflexes in the human vestibular system, in which VOR reflects the dynamic vestibular function. The semicircular canals in the inner ear provide sensory input on head velocity, which enables the VOR to generate eye movement that is conjugated with head movement. The desired result is that the subject’s eyes keep fixating to the target during any motion of the head, enabling clear vision. Consequently, VOR gain is a decisive factor in the otology department. In order to measure this dynamic vestibular function specifically, it is necessary to use high-acceleration examination of the patient, and one of those examinations is the head impulse test (HIT). In an HIT, the clinician briskly rotates the subject’s head while the subject is gazing at a target. Each impulse is supposed to be unpredictable for the subject at low amplitude (15°-30°), high velocity (200-400 (°)/s), and high acceleration (2000-4000 (°)/s2). In response to these high-acceleration movements of the head, the subject’s vestibular system will provide compensatory eye movement in order to keep the eyes gazing at the target. Consequently, VOR gain is calculated by taking a ratio of eye-to-head kinetic characteristics, mainly position gain and velocity gain. The normal range of VOR gain is 0.7-1.0, lower gain related to VOR function loss [1-7].
Over the past decade, the search coil method has been used to perform the HIT. This test, however, is replaced by video HIT (vHIT), which offers more convenience to both patients and clinician because done at the bedside, it is of short-duration, and applicable to patients with acute vestibular neuritis and efficient in identifying peripheral vestibular deficits compared with the search coil method. Another advantage of vHIT compared to the conventional head impulse test is that it enables the clinician to see some unconscious invisible pursuits during the head impulse, called covert catch-up saccade, which might lead to a different diagnosis [4, 8].
One of the most challenging tasks clinicians are confronting with is to combine all the results from different check-ups of the patient, convergent to a diagnosis. In the otology department, patients undergo several examinations, such as the head impulse test, and the caloric test. Afterwards, the examiners and doctors analyze these medical data based on human knowledge and reasoning, in order to inform patients about their corresponding physical condition. Therefore, a collaborative application that is able to analyze patient’s medical data and predict their unknown patterns is more accommodating, and in some ways, crucial [9].
Fuzzy logic is an extension of Boolean logic based on the mathematical theory of fuzzy sets. By introducing fuzziness, called the membership function, thus enabling a conditional state other than just true or false, fuzzy logic provides valuable and flexible reasoning, which makes it possible to take into account inaccuracies and uncertainties. One advantage of using fuzzy logic to formalize human reasoning is that its rules are set in natural language. That is why fuzzy logic is applicable for constructing a human-readable collaborative recommendation application [9].
The goal of our study was to propose a new fuzzy- logic recommendation stand-alone application that is autonomous and collaborative with the user by providing useful information and recommendations about the subject’s condition and how it is related to other examinations, such as the caloric test. The first experiment provided useful information on the comparison between position gain and velocity gain, covert catch-up saccade analysis, and covert catch-up saccade-removed VOR gain. Afterwards, the calculated covert catch-up saccade and position gain were used as input to the recommendation application.
2 Experiments
2.1 Subjects and measurements
2.1.1 Subjects
Seven subjects were recorded with vHIT. All seven patients had acute unilateral peripheral vestibulopathy diagnosed from clinical symptoms and a vestibular function test (mean 46 years, age range 22-69, and one female).
2.1.2 Measurements
Excel files of subject data were exported from ICS Impulse (GN Otometrics A/S, Hoerskaetten 9, DK-2630 Taastrup, Denmark), and then analyzed offline by Mathworks MATLAB R2012a and Microsoft Excel 2013.
2.2 Experiment 1
2.2.1 Video head impulse test data
BARIN [10] reported that lateral vHIT responses for head velocities below 100 (°)/s are not a test of VOR, because other responses will be involved when head velocity is less than 100 (°)/s. In addition, the maximum velocity of head thrust should be less than 250 (°)/s for patient safety. For vertical planes, vHIT responses for head velocities below 50 (°)/s are mediated entirely by the oculomotor system, which means that VOR does not play any role. As a result, lower limit of head velocity for vertical planes is 50 (°)/s and recommended upper limit is 200 (°)/s for patient safety. Therefore, the clinician must perform the thrust is in the range of 100 to 250 (°)/s for lateral vHIT and 50-200 (°)/s for vertical vHIT.
Figure 1 represents one single lateral vHIT thrust. Head velocity trace is characterized and almost analogous by the clinician’s handwork, normally in the range of 100-250 (°)/s as mentioned above. Patients with different physical conditions will give different responses to equal head thrust. As shown in Fig. 1, the eye pursuit curve contains one eye response peak, one covert catch-up saccade, and the last peak which can be overt catch-up saccade or spontaneous nystagmus.
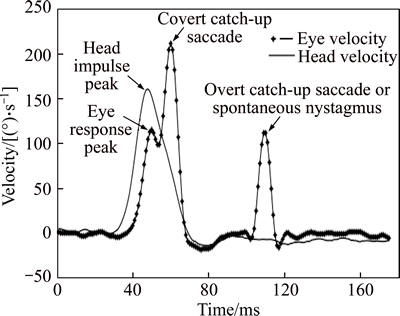
Fig. 1 Video head impulse test data
2.2.2 Methodology
After being recorded with vHIT, the subjects’ data were processed offline with MATLAB software. As mentioned above, VOR is calculated by taking a ratio of eye-to-head kinetic characteristics. To be more specific, position gain and velocity gain are two main calculations for VOR, in which position gain is the total degree of eye rotation divided by the total degree of head rotation from the start of the thrust until the start of a covert catch-up saccade [2]. Nevertheless, in this work, position gain calculation was optimized by removing covert catch-up saccade, if there was any, namely, the desaccade method.
On the other hand, velocity gain as the ratio of mean eye velocity to mean head velocity during a 40 ms window is centered on peak head acceleration [4]. The normal VOR gain (in both velocity gain and position gain) is expected to be higher than 0.7; otherwise, there is vestibular loss [1].
Gain asymmetry, was calculated as follows [3]:
 (1)
(1)
where GRight is the rightside gain and GLeft is the leftside gain.
For gain asymmetry, the criterion for normal data is considered to be less than 5.6%; otherwise, the results are abnormal.
2.2.3 Statistical analysis
In Table 1, for seven subjects, for ipsilesional and contralesional sides, position gain (0.94±0.17) was higher than velocity gain (0.84±0.19.)
On the other hand, gain asymmetry of both lesion and intact sides using velocity gain was higher than that from using position gain (four out of five subjects; two subjects (both RtCP29% VN[R]) were excluded because their gain asymmetry was not significant). In Fig. 2, position gain asymmetry and velocity are represented.
For subjects diagnosed with unilateral vestibular neuritis, velocity gain might depict vestibular weakness more effectively than position gain. In Fig. 2, for subjects who had high gain asymmetry, one with low unilateral vestibular weakness had position GA of 15.9% and velocity GA of 12.0%; four others with high unilateral vestibular weakness had position GA of (16.5±5.66)% and velocity GA of (22.7±8.93)%. On the other hand, two low gain asymmetry subjects had position GA of (0.96±0.02)% and velocity GA of (0.25±0.35)%.
2.2.4 Covert catch-up saccade
During the head impulse test, some adaptive eye responses might occur to provide more compensatory pursuit to head movement. They are catch-up saccades, with one type named overt catch-up saccades, which are direct, happen after the head rotation, and are visible to the clinician; the other is covert catch-up saccades, which are indirect, happen during head rotation, and are invisible to the clinician. Another motor response, which appears in vHIT eye velocity, is spontaneous nystagmus. This is rapid involuntary movement of the eyes, and is mainly caused by a central lesion [8]. In this work, a spontaneous nystagmus was ignored and grouped with overt catch-up saccades for further examination.
Physiological saccades were identified based on their peak eye velocity (60±19) (°)/s and occurred with a latency of (215±38) ms after onset of vHIT. Refixation saccades were measured at an average latency of (146±28) ms (covert saccades) and (245±48) ms (overt saccades). Peak eye velocity of refixation saccades was (249±51) (°)/s for covert saccades and (148±81) (°)/s for overt saccades, respectively [11].
As shown in Fig. 1, in this work, eye response peak is defined as the first maxima peak of eye response after head impulse peak. The minima right after the eye response peak, called the response valley, were also calculated and used to distinguish covert catch-up saccades and overt catch-up saccades. Covert catch-up saccades were detected by the first maxima after the eye response peak if the valley did not reach zero; otherwise, they were overt catch-up saccades or a spontaneous nystagmus.
2.3 Experiment 2
The data in Experiment 1 were fed into a recommendation stand-alone application as input, the purpose being to get a recommendation summary. The recommendation application uses weighted fuzzy logic.
Figure 3 shows the application flowchart consisting of three main parts: clinician, data transfer and application. First, the vHIT data are obtained from the video head impulse test, exported to a .csv file, and fed to the application as input. In the main application, covert catch-up saccade occurrence and position gain were calculated. Subsequently, these factors were used as input to the recommendation application to get the efficiency as output. This output, consisting of a report chart and report menu, is packed and sent back to the clinician. Based on the received report, the clinician can render a decision as to the patient’s condition.
2.3.1 Position gain calculation
The whole data set is divided into three sets: normal, covert catch-up saccades (the covert set), and overt catch-up saccades and spontaneous nystagmus (the overt set). In this work, a spontaneous nystagmus was treated as an overt catch-up saccade.
Normal eye movements are defined as eye movements that do not contain any type of catch-up saccade, as well as spontaneous nystagmus.
Table 1 Comparison of position gain and velocity gain, and gain asymmetry
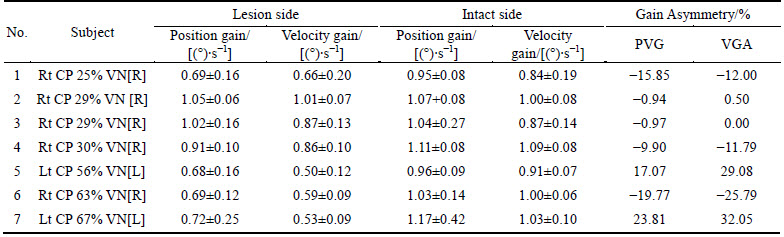
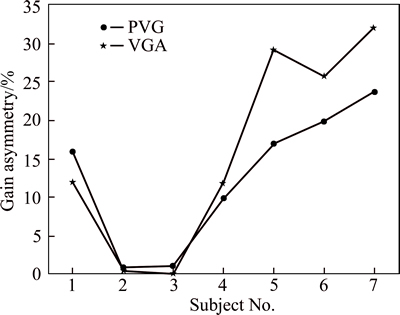
Fig. 2 Position gain asymmetry and velocity gain asymmetry
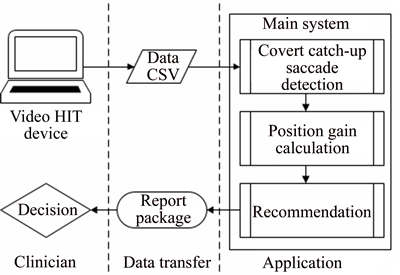
Fig. 3 System flowchart
The remaining sets were divided into the covert set and overt set based on the valley of eye movement after the eye response peak, defined as the response valley. By using zero crossing, if this valley reaches zero before the next maxima of eye movement, the data are grouped into the covert set; otherwise, into the overt set.
For the normal set and overt set, the position gain is the ratio of head movement, area under the head velocity curve from its onset to zero crossing, to eye movement, area under the eye velocity curve from its onset to next-first zero crossing.
For the covert set, at first, desaccade is applied by replacing covert catch-up saccade by the short line, from its response valley to its next first zero-crossing. Afterward, position gain is calculated as the ratio of head movement, area under the head velocity curve from its onset to zero crossing, to eye movement, area under the eye velocity curve from its onset to next-first zero crossing.
2.3.2 Recommendation application
Fuzzy logic is a non-linear mapping of crisp input into corresponding crisp output by using linguistic knowledge. The conventional fuzzy logic system is comprised of five main procedures: fuzzification, fuzzy operator application, implication operation application, output aggregation, and finally, defuzzification.
In this experiment, fuzzy logic was used to convert position gain and appearance of covert catch-up saccades (from Experiment 1) into the efficiency of the subject’s vestibule function, which is more significant to the application user.
This application consists of two recommendation applications. Mainly, these two applications are a Mamdani type, where the implementation method is minimum, the aggregate method is maximum, and defuzzification is the minimum of the maximum. The first is Recommendation 1, one input for which is the position gain. The second is Recommendation 2, with two inputs: position gain and appearance of covert catch-up saccade.
1) Recommendation 1
The purpose of the design for the Recommendation 1 application is to reduce the confusion of variety in VOR gain. Within one examination, VOR gain can vary from a small range to a very large scale. This problem is usually solved with the instruments by using an outlier-removing method, during and after examination, or intuitive and manual impulse deletion by the clinician after receiving the results. After removing outliers, the instrument automatically calculates the mean gain and saves it as the patient’s report, without knowing how the outlier quantity should be removed. The recommendation application provides a different viewpoint; it eliminates the uncertainty of position gain by obtaining a fuzzy value from the crisp position gain.
As shown in Fig. 4, the crisp set position gain ([0, 3]) is divided into three subsets, LowGain [0 0.9], NormalGain [0.5 1.5], and HighGain [1 3]. All subsets’ membership function is a trapezoidal function over a range or position gain. Meanwhile, the output is set with two other trapezoidal functions: Abnormal [0 0.9] and Normal [0.1 1], as shown in Fig. 5. Subsequently, three rules are simply applied as follows: (1) If (Gain is LowGain) then (Response is Abnormal), weighted 0.7; (2) If (Gain is NormalGain) then (Response is Normal), weighted 0.8; (3) If (Gain is HighGain) then (Response is Abnormal), weighted 0.5.
Finally, Fig. 6 shows the fuzzy application input– output relationship, which is more flexible than under conventional analysis. Without this recommendation application, this relationship is simply a step function, in which normal response is set in the range of [0.70, 1.00] of VOR gain, with lower or higher gain considered to be abnormal response.
2) Recommendation 2
The second recommendation, Recommendation 2, will give the clinician a different output after combining catch-up saccade occurrence and position gain.Recommendation 2 requires one more input of covert catch-up saccade detection.
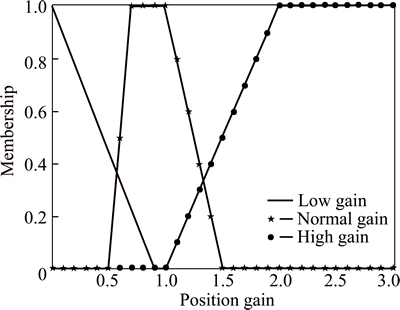
Fig. 4 Input membership function of Recommendation 1 (This membership function consists of three trapezoidal functions, LowGain [0 0.9], NormalGain [0.5 1.5], and HighGain [1 3])
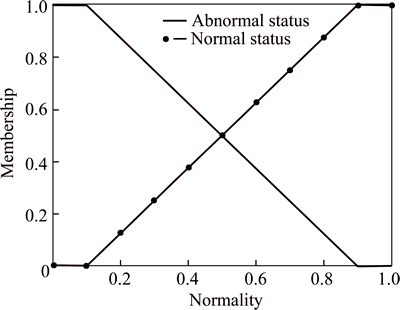
Fig. 5 Output membership function of Recommendation 1 (This membership function consists of two trapezoidal functions, Abnormal [0 0.9] and Normal [0.1 1])

Fig. 6 Input-output relationship of Recommendation 1
As shown in Fig. 7, the membership function of CovertCatch-up saccade has simply two values, No ([0]) and Yes ([1]). The membership of position gain input and output is the same as the Recommendation 1 structure. Nonetheless, six rules are designed to adapt two inputs: (1) If (Gain is LowGain) then (Response is Abnormal)weighted 0.7; (2) If (Gain is NormalGain) and (CovertCatchup is No) then (Response is Normal) weighted 1; (3) If (Gain is HighGain) then (Response is Abnormal) weighted 0.5; (4) If (Gain is LowGain) and (CovertCatchup is Yes) then (Response is Abnormal) weighted 1; (5) If (Gain is HighGain) and (CovertCatchup is Yes) then (Response is Abnormal) weighted 1; (6) If (CovertCatchup is Yes) then (Response is Abnormal) weighted 0.8.

Fig. 7 Input membership function of Recommendation 2 (This membership function consists of two sharp triangle functions, centered at 0 (No), and 1 (Yes))
3 Discussion
In the first experiment, for ipsilesional and contralesional sides, the calculated position gain (0.94±0.17) was higher than velocity gain (0.84±0.19). Moreover, for acute unilateral peripheral vestibulopathy subjects, gain asymmetry of both lesion and intact sides using velocity gain is mostly higher than that from using position gain (four out of five subjects).
The results obtained from Recommendation 1 are shown in Fig. 8. The input of this application is vHIT data of one subject, which contains 28 left-hand side impulses. The smoothed line indicates the calculated position gain, (0.82±0.26), while the fuzzy output is definitely divided into two ranges: one with (0.31±0.02), which indicates a low efficiency of 31%; the second range is (0.90±0.07), which indicates normal efficiency of 90%. Therefore, with this recommendation application, the clinician is provided with efficiency instead of a crisp position gain value.
Figure 9 shows the input-output relationship of Recommendation 2 in three dimensions because there are two inputs. The result obtained from Recommendation 2 is shown in Fig. 8 and in the Report Menu in Fig. 10. There are 11 impulses with occurrence of covert catch-up saccades, with corresponding efficiency dramatically decreasing to 0.125. This result is crisp, but somehowrepresents the effect of covert catch-up saccades on the diagnosis decision. In order to improve this result, a new membership function for CovertCatchup input should be implemented. The Report Menu in Fig. 10 shows detected strange pursuits, such as covert catch-up saccade, overt catch-up saccade, spontaneous nystagmus, or just a normal impulse.
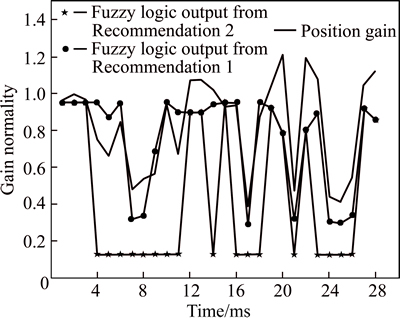
Fig. 8 Recommendation system output
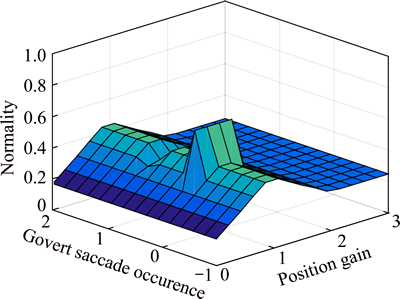
Fig. 9 Input-output relationship of Recommendation 2
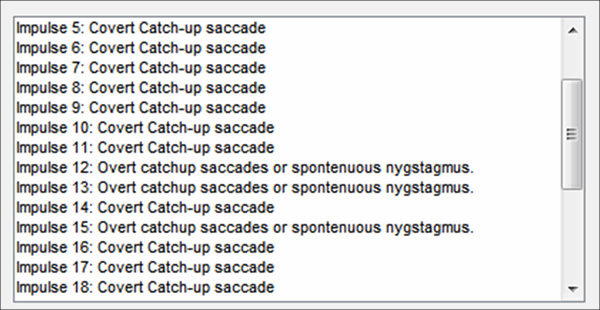
Fig. 10 Report menu of Recommendation 2
4 Conclusions
In the first experiment, for ipsilesional and contralesional sides, the calculated position gain (0.94±0.17) was higher than velocity gain (0.84±0.19). Moreover, for acute unilateral peripheral vestibulopathy subjects, gain asymmetry of both lesion and intact sides using velocity gain is mostly higher than that from using position gain (four out of five subjects). Hence, gain asymmetry using velocity gain might depict vestibular weakness better than position gain. Consequently, our suggestion is that, position gain, velocity gain, and gain asymmetry should be included in the clinical diagnosis.
In the first experiment, covert catch-up saccades and desaccaded position gain are calculated. These data were used as input to a recommendation system, which is collaborative with the clinician to obtain a better diagnosis statement. This recommendation system consists of two subsystems. The one-input Recommendation 1 provides the efficiency of each impulse’s response, whereas the two-input Recommendation 2 gives different output caused by covert catch-up saccade occurrence. The purpose of the design for the Recommendation 1 system is to reduce the confusion of variety in VOR gain and to provide more efficiency rather than a crisp position gain value to the clinician.
The second system, Recommendation 2, gives the clinician different output after combining catch-up saccade and position gain. Recommendation 2 requires one more input of covert catch-up saccade detection. Output of this system is crisp, but somehow represents the effect of covert catch-up saccades on diagnosis decision.
In future work, a new membership function for CovertCatchup input will be implemented to obtain the output that is more precise. In addition, weighted fuzzy logic will be applied to get higher accuracy in reasoning by combining overt catch-up saccades, covert catch-up saccades, and other lab-test results.
Acknowledgment
This research was supported by the MSIP (Ministry of Science, ICT and Future Planning), Korea, under the ITRC (Information Technology Research Center) support program (IITP-2016-H8501-16-1019) supervised by the IITP (Institute for Information & Communications Technology Promotion) and Inha University Research Grant. And it was also supported by the Basic Science Research Program through the National Research Foundation (NRF) of Korea funded by the Ministry of Education (2010-0020163).
References
[1] CREMER P, HALMAGYI G, AW S, CURTHOYS I, MCGARVIE L, TODD M, HANNIGAN I. Semicircular canal plane head impulses detect absent function of individual semicircular canals [J]. Brain, 1998, 121: 699-716.
[2] ROY F D, TOMLINSON R D. Characterization of the vestibulo- ocular reflex evoked by high-velocity movements [J]. Laryngoscope, 2004, 114: 1190-1193.
[3] WEBER K P, AW S T, TODD M J, MCGARVIE L A, CURTHOYS I S, HALMAGYI G M. Head impulse test in unilateral vestibular loss- vestibulo-ocular reflex and catch-up saccades [J]. Neurology, 2008, 70(6): 454-463.
[4] MACDOUGALL H G, WEBER K P, MCGARVIE L A, HALMAGYI G M, CURTHOYS I S. The video head impulse test diagnostic accuracy in peripheral vestibulopathy [J]. Neurology, 2009, 73(14): 1134-1141.
[5] MACDOUGALL H G, MCGARVIE L A, HALMAGYI G M, CURTHOYS I S, WEBER K P. The video head impulse test (vHIT) detects vertical semicircular canal dysfunction [J]. PLoS One, 2013, 8(4): e61488.
[6] PALLA A, STRAUMANN D, OBZINA H. Eye-position dependence of three-dimensional ocular rotation-axis orientation during head impulses in humans [J]. Experimental Brain Research, 1999, 129(1): 127-133.
[7] WEBER K P, MACDOUGALL H G, HALMAGYI G M, CURTHOYS I S. Impulsive testing of semicircular-canal function using video-oculography [J]. Basic and Clinical Aspects of Vertigo and Dizziness, 2009, 1164: 486-491.
[8] HERDMAN S J. Vestibular rehabilitation [M]. Georgia: Contemporary Perspectives in Rehabilitation. 2007.
[9] MENDEL J. Fuzzy-logic systems for engineering-A tutorial [J]. Proceedings of the IEEE, 1995, 83(3): 345-377.
[10] BARIN K. Video head impulse testing (vHIT): A novel test for peripheral vestibular disorders [C]// 15th Workshop on Neurotology and Medical Audiology. 2014.
[11] BLOEDOW A, PANNASCH S, WALTHER L E. Detection of isolated covert saccades with the video head impulse test in peripheral vestibular disorders [J]. Auris Nasus Larynx, 2013, 40(4), 348-351.
[12] MILES R. VorteqTM VHIT [M]. Micromedical Technologies, 2013.
[13] REY-MARTINEZ J, BATUECAS-CALETRIO A,  E, FERNANDEZ N P. HITCal: A software tool for analysis of video head impulse test responses [J/OL]. Informa Healthcare, 2015. doi: 10.3109/00016489.
E, FERNANDEZ N P. HITCal: A software tool for analysis of video head impulse test responses [J/OL]. Informa Healthcare, 2015. doi: 10.3109/00016489.
[14] HUSSEIN A S, OMAR W M, ATI X L M. Accurate and reliable recommender system for chronic disease diagnosis [C]// 1st International Conference on Global Health Challenges. 2012.
[15] KAWAMOTO K, HOULIHAN C A, BALAS E A, LOBACH D F. Improving clinical practice using clinical decision support systems: A systematic review of trials to identify features critical to success [J]. British Medical Journal, 330(7494), 765.
[16] DERNONCOURT F. Fuzzy logic: Introducing human reasoning within decision-making systems?[C]// Conservatoire National des Arts et Métiers. Paris, 2011.
[17] ROSS J T. Fuzzy logic with engineering applications [M]. Great Britain: John Wiley & Sons, Ltd. 2010.
[18] HINES J W. MATLAB supplement to fuzzy and neural approaches in engineering [M]. A Wiley-Interscience Publication: John Wiley & Sons, Inc. 1997.
(Edited by YANG Bing)
Received date: 2015-06-12; Accepted date: 2016-02-23
Corresponding author: KWON Jang Woo, Professor, PhD; Tel: +82-32-860-7443; Email: jwkwon@inha.ac.kr
Abstract: Vestibulo-ocular reflex (VOR) is an important biological reflex that controls eye movement to ensure clear vision while the head is in motion. Nowadays, VOR measurement is commonly done with a video head impulse test based on a velocity gain algorithm or a position gain algorithm, in which velocity gain is a VOR calculation on head and eye velocity, whereas position gain is calculated from head and eye position. The aim of this work is first to compare the two algorithms’ performance and to detect covert catch-up saccade, then to propose a stand-alone recommendation application for the patient’s diagnosis. In the first experiment, for ipsilesional and contralesional sides, the calculated position gain (0.94±0.17) is higher than velocity gain (0.84±0.19). Moreover, gain asymmetry of both lesion and intact sides using velocity gain is mostly higher than that from using position gain (four out of five subjects). Consequently, for subjects who have unilateral vestibular neuritis diagnosed from clinical symptoms and a vestibular function test, vestibular weakness is depicted by velocity gain much better than by position gain. Covert catch-up saccade and position gain then are used as inputs for recommendation applications.


